Remember, if you can, back to the long-ago world of March 2020: Many of us were new to videoconferencing or used it only occasionally. Almost instantly, however, our schedules filled with virtual work meetings, virtual exercise classes and virtual get togethers. Today, almost a year into COVID-19-induced social distancing, videoconferencing has become woven into the fabric of our everyday lives.
It may have taken a pandemic to convert Americans to the convenience of videoconferencing, but now we’re all in. The same can be said for telehealth. After years in which telemedicine’s promise was hampered by a widespread lack of adoption in the U.S., the coronavirus gave Americans what even the smartest telemedicine marketing could not: a compelling reason to shift certain kinds of care from in-person to virtual, and according to a Rally Health survey focused on preventive care, one in three Americans plan to continue scheduling telemedicine appointments when possible even after COVID-19 is no longer an issue.
Hurry Up and Wait
Over the past decade, telehealth—the umbrella term used to describe all medical services and health education delivered digitally—has grown to a $45.5 billion industry, according to data from Global Market Insights. Still, many patients weren’t clear how much they’d be charged for a virtual visit or whether it would be covered by insurance; they didn’t know how to sign up for one; and they wanted to maintain their relationship with their regular physician, who likely wasn’t offering virtual services.
That all changed in March, when many doctors urged patients with non-emergent needs to postpone in-person care as the COVID-19 pandemic spread. In 2020, virtual visits were on pace to top 1 billion, according to Forrester analysts. What’s more, a whopping 84% of patients seeking virtual care in March last year were doing so for the first time, according to an IDC report.
Sudden efforts to digitize health care delivery were aided by state and federal authorities that quickly loosened telehealth licensing restrictions and by changes to Medicare and Medicaid that began to reimburse providers for a far wider swath of telehealth services. The CDC and WHO, meanwhile, began advocating for telemedicine, while the American Medical Association released new guidelines to help providers get up to speed.
A study led by researchers at NYU Grossman School of Medicine highlights the degree to which traditional health care providers have extended their reach through virtual visits. Between early March and mid-April last year, researchers found that virtual urgent care visits to NYU Langone Health grew by 683%, while non-urgent virtual visits mushroomed by a previously inconceivable 4,345%. OptumCare quickly went from 1,000 providers using telemedicine before the pandemic to more than 14,000 using it today. At a time when clinicians risked losing contact with quarantined patients, it became clear that telemedicine offered a powerful new way to connect.
A Case Study: Diabetes
Just as telehealth picked up steam, early COVID-19 research also revealed the outsized impact of the virus on higher-risk populations, including those with obesity or diabetes. Given diabetics’ increased risk and their established success with other digital health interventions, such as continuous glucose monitors, the pandemic offers a unique opportunity to push digital education, prevention and maintenance tools onto the centerstage of diabetes care.
The grim statistics show why diabetics need robust digital health support. Reports from the Centers for Disease Control and Prevention (CDC) and other national health centers and hospitals, for example, have shown that the risk of a fatal outcome from COVID-19 is up to 50% higher in patients with diabetes than in those who do not have diabetes. What’s more, there are now 34 million diabetic adults in the United States, representing 13% of the population. More than 7 million of them meet the clinical definition of diabetic, but don’t realize they have the disease, according to the CDC. Even more shocking: 88 million Americans—nearly 1 in 3—have prediabetes, a condition that puts people at significantly higher risk of developing Type 2 diabetes, as well as stroke and heart disease. And the vast majority of prediabetics—90%—don’t realize they have the condition. The fact that so many diabetic and prediabetic Americans are oblivious to their condition makes proactive prevention and lifestyle adjustments all the more imperative.
There is some good news: Just as Americans embraced Zoom exercise classes and virtual doctor visits, they have also flocked to technology-enabled tools to take control of their weight, nutrition and activity levels—all of which are crucial to diabetes prevention. Now, as so many people embrace new health technology, we have the perfect opportunity to implement widespread digital diabetes prevention initiatives and improve our chances of fighting this health crisis.
Digital Toolbox
Even before we retreated to our homes, Americans had grown increasingly comfortable with digital tools, from wearable activity monitors to online scheduling apps. But, we know that the best virtual health services combine the power of always-on, automated technology with the warmth and encouragement that only a real person can offer.
Decades of research have shown us that small, specific and easy-to-execute actions create the best chance of long-term habit formation—and social support keeps us going as we create fresh patterns. From virtual weight-loss and smoking-cessation coaching to video appointments with mental health counselors, our connected world can now deliver immediate access to live professionals who help reassure, focus and motivate us as we work to adapt to a new lifestyle; control the factors within our control; and take the next step toward building healthy habits. The sudden onset of a worldwide pandemic and social distancing served to reinforce these truths and prove that virtual health not only works but works at scale.
After months of getting used to this new normal and relying on virtual connections to aid our health, we’re not about to give them up. Now that millions of Americans have navigated their first telehealth visit—and millions more have tapped online and mobile health tools to create new, grounding routines—we’ve finally realized just how beneficial ongoing digital health care can be, even as we look ahead to a post-pandemic world.
The New New Normal
We’ve reached a critical inflection point for diabetes prevention and management: We must maintain the momentum that telemedicine and digital health have gained over the last year by continuing to make virtual services readily available. For that to happen, the government will need to extend its earlier flexibility, which paved the way for reimbursement, and create incentives for providers to maintain a telehealth presence beyond the pandemic. We also must continue to do better for people facing chronic health conditions by creating new ways for them to connect with professionals and create sustainable lifestyle changes.
Happily, telemedicine is well along in its ascent. The industry is poised to nearly quadruple to more than $175 billion by 2026, according to Global Market Insights. The American Telemedicine Association predicts that 50% of health care services in the U.S. will be conducted virtually by 2030.
"Now that patients and health care providers alike are experiencing telehealth, there will be no turning back," Ann Mond Johnson, CEO of the ATA, recently told ABC News. "And as we come out of this health crisis, telehealth will be a mainstay of our system and accepted for what it is—not telehealth, but health.
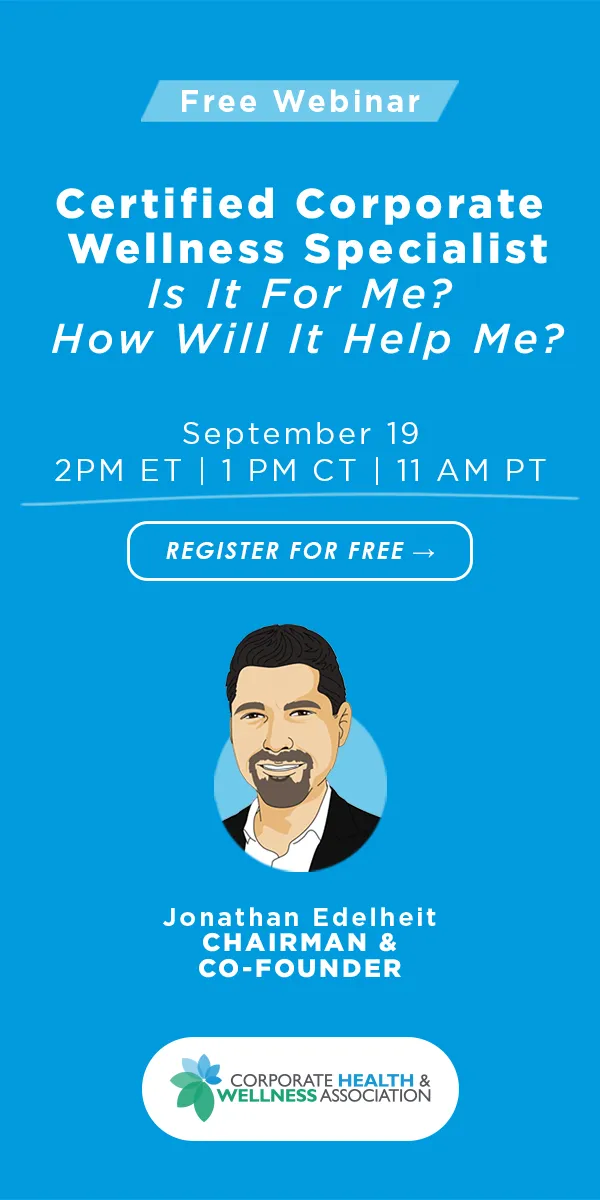
With telehealth on the rise, employers will need to pivot their employee health strategies. Attending the virtual conference, Healthcare Revolution, will help give you the ins and outs of virtual health directly from industry leaders.